How ai and artificial intelligence can streamline administrative tasks in the health system
AI can streamline a broad scope of work in the health system. First, it reduces time spent on documentation, billing, scheduling, claims, and patient communications. Second, it improves data quality and lowers error rates when clinicians capture notes or when staff complete forms. Also, AI helps with triage and routine replies so clinicians regain time and attention for direct care. For example, an ambient AI scribe can transcribe visits immediately, and then the clinician edits instead of typing long notes. In that way, AI to process notes shortens hours at the chart and helps reduce physician burnout.
Furthermore, the multifaceted role of AI includes tools that auto-populate EHR fields, flag inconsistent entries, and suggest appropriate procedure codes. Consequently, claim denials drop and billing cycles shorten. Additionally, AI algorithms can classify incoming messages and route them to the right team. Thus, shared mailboxes become manageable and staff respond faster. Our customers note substantial reductions in manual copy-paste and context hunting thanks to integrated agents like virtualworkforce.ai that draft accurate, context-aware replies inside Outlook and Gmail.
In practice, the use of artificial intelligence extends beyond simple automation. For example, large language models can summarize patient histories, while machine learning predicts no-shows and optimizes appointment slots. Also, AI can surface actionable insights from a dataset of past cases to speed decisions. To be clear, automation does not remove human judgment. Instead, AI offers suggestions and triage, and staff handle exceptions. This hybrid model helps work smarter and reduces repetitive clerical burden.
Evidence supports this approach. The American Medical Association reports that many clinicians identify reducing administrative burden as the top benefit of AI in practice; clinicians believe AI can enhance the time they spend with patients and the quality of care (American Medical Association). In short, AI offers precise ways to automate routine work and to enhance clinical time. Next, we look at how to quantify those gains and build a business case for investment.

Quantifying time on administrative and admin work: survey evidence (122 hours, 57%)
Quantifying time on administrative duties gives leaders the evidence they need to invest in AI. For instance, a recent pilot showed workers could save about 122 hours per year by letting AI handle administrative emails and scheduling. Also, a survey found that 57% of physicians put reducing administrative burdens at the top of AI priorities. Therefore, leaders should measure hours saved, claim denial rates, appointment fill rates, and clinician time with patients to make a convincing business case.
To start, define a baseline metric. First, capture average time per admin task and the total number of such tasks per clinician per week. Second, track claim denial rates and rework. Third, look at inbox metrics like average response time and number of threads per case. Then apply an AI pilot to a controlled group and compare results. For example, measure reductions in time spent on data entry and the percentage of emails resolved without human escalation. These are clear, actionable metrics that board members understand.
Additionally, workforce studies show shifts in office roles tied to automation. Some employers expect changes in staffing for clerical positions as AI scales; this reality makes the case for retraining and redeployment rather than layoffs (National University). Also, projections suggest pressure on office roles as automation improves. Therefore, include transition costs and training in the ROI model. Finally, quantify secondary gains such as lower physician burnout and improved patient throughput. When you present these combined metrics—time saved, revenue cycle improvements, clinician satisfaction—you create a robust argument for adoption.
Drowning in emails?
Here’s your way out
Save hours every day as AI Agents label and draft emails directly in Outlook or Gmail, giving your team more time to focus on high-value work.
ai tool and ai systems to optimize data management and inbox workflows
Implementing the right AI tool matters. Tools like Dragon Medical One speed clinical documentation with speech-to-text while RPA handles billing and claims automation. Also, platforms that fuse email history with ERP or EHR data bring context to replies. For example, virtualworkforce.ai integrates ERP and email memory to draft reply-first emails and to update systems, so teams cut handling time dramatically. Use AI systems that provide role-based access, audit logs, and redaction to keep sensitive information safe.
Practical wins include auto-populating records, triaging inbox messages, and reducing duplicate entry. First, an AI-powered message triage filters low-priority threads and surfaces urgent items to clinicians. Second, a no-code AI agent can draft templated responses that cite source systems and attach the right documents. Third, automation of claim scrubbing removes common coding errors before submission. To ensure success, verify vendor integration with your EHR and APIs. Also, test on a representative dataset and validate outputs against clinician review.
When evaluating vendors, use a checklist. Ask if the solution offers an ambient AI scribe, supports custom connectors, and provides a clear escalation path. Next, confirm logging and human-in-the-loop controls. Also, determine how much prompt tuning or configuration is needed. For many ops teams, no-code options speed rollout and reduce reliance on prompt engineering. If you want a logistics-minded approach to email automation inside Outlook or Gmail, see our guide on automated logistics correspondence for similar techniques and integration patterns (automated logistics correspondence).
Ultimately, choose AI solutions that reduce repetitive tasks and that enhance data management. Also, ensure they can integrate with existing workflows and that stakeholders control behavior. This approach helps teams scale while protecting clinical safety and privacy.
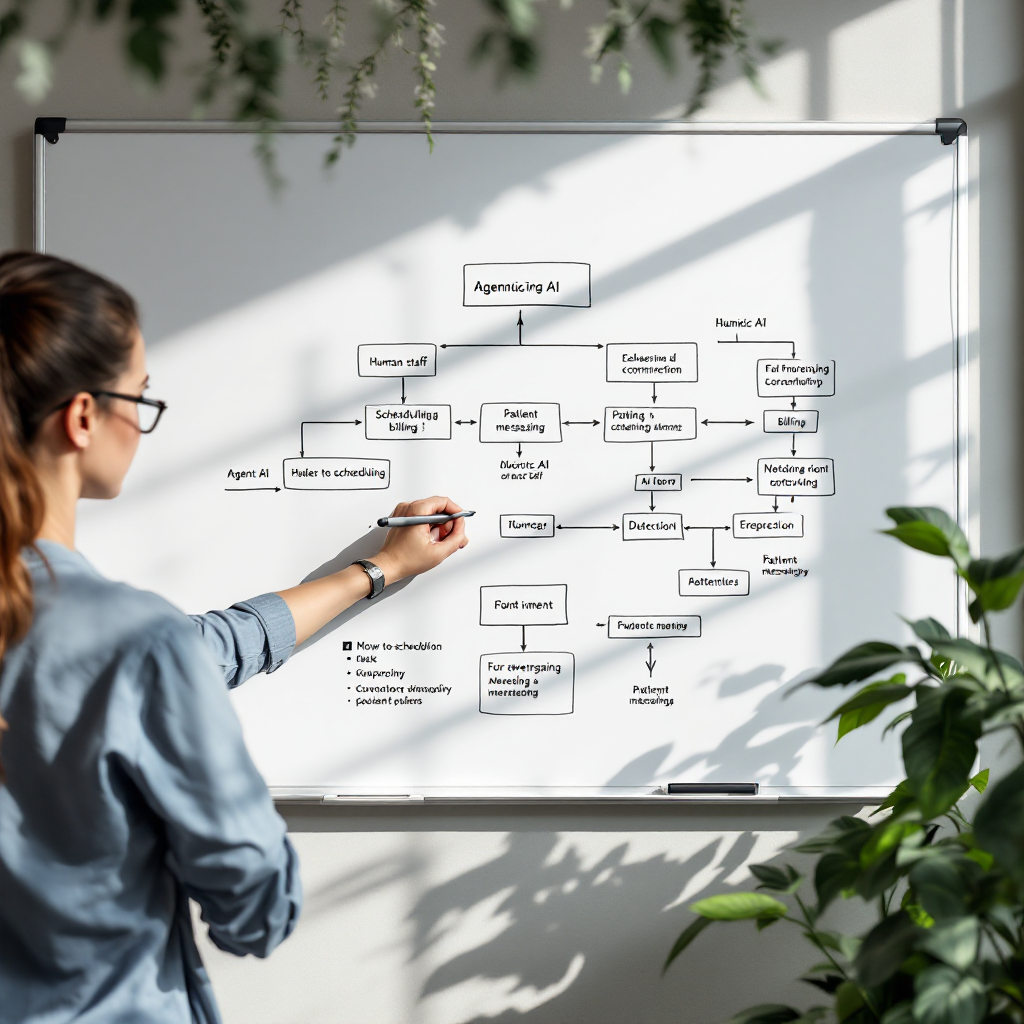
automation, agentic ai and ai at work: redesign workflow and resource allocation to reduce administrative burden
Redesigning workflow matters as much as technology. Where automation fits depends on the task. Rule-based RPA works well for predictable billing steps. Machine learning supports coding suggestions and fraud detection. Meanwhile, agentic AI can coordinate multi-step processes like authorizations by calling APIs, drafting messages, and escalating exceptions. These agents work best where rules and data provide clear guidance and where human review covers edge cases.
Start by mapping current steps and time per step. Then identify which tasks to automate, which to augment with AI, and which to retain for human judgment. For example, shift approvals and routine scheduling to AI agents while clinicians handle clinical decisions. This shift improves resource allocation and reduces clinician administrative burden. Next, reassign freed hours to care delivery, quality improvement, education, or staff retraining. That approach turns time savings into better care rather than headcount reductions alone.
Also, define exception handling clearly. For routine cases, let AI finalize the action. For ambiguous cases, route to a specialist or use a human-in-the-loop rule. Use metrics to monitor accuracy, and adjust thresholds to balance speed and safety. Furthermore, consider impacts on workload distribution: as AI takes over repetitive inquiries, staff can focus on tasks that improve patient experience. To explore how email automation can scale without hiring, review our playbook for scaling logistics operations with AI agents (how to scale logistics operations with AI agents).
Finally, workforce planning should include retraining and role redesign. Rather than only cutting roles, redeploy staff into higher-value functions such as care coordination. This way, AI helps to optimize resource allocation and to enhance productivity across teams. The opportunity for AI is to free time for clinicians and to improve system throughput while keeping safety and accountability front and center.
Drowning in emails?
Here’s your way out
Save hours every day as AI Agents label and draft emails directly in Outlook or Gmail, giving your team more time to focus on high-value work.
Responsible ai adoption: addressing administrative risks, prompt engineering and governance so ai to deliver value
Responsible AI adoption requires governance and careful testing. First, manage risks like data quality, privacy, bias, and auditability. Second, ensure logging and traceability so every output links to source data. Third, put human reviewers in place for clinical safety and for high‑risk decisions. These steps protect patients and reduce legal exposure.
Also, build standard prompt templates and guardrails to keep outputs consistent. Prompt engineering helps, but so do configuration options that let operations set tone, templates, and escalation paths without deep technical work. For vendors that offer no-code setup, this reduces dependence on AI training specialists and speeds rollout. Additionally, maintain a dataset for ongoing validation and monitor drift. Regularly retrain models where needed and keep a change log for audits.
Governance essentials include testing on representative clinical data, role-based access to sensitive records, and a clear incident response plan. Furthermore, require vendors to support audit exports and to document algorithmic behavior. For transparency, publish high-level descriptions of how AI was trained and validated, while protecting proprietary details. Finally, involve clinicians and compliance teams in every stage so the use of artificial intelligence aligns with clinical standards and regulations.
To manage adoption risks, define KPIs early. Track error rates, escalation volumes, and the impact on time on administrative tasks. Also, evaluate the impact on physician burnout and on billing accuracy. This disciplined approach ensures AI offers measurable value and that teams can trust ai-powered software in daily operations.
How to embrace ai and use ai to enhance productivity, optimise resource allocation and accelerate adoption across the health system
Embrace AI with a clear pilot-to-scale pathway. First, pick a use case with strong ROI and measurable outcomes. Second, run a narrow pilot, measure improvements, and iterate. Third, scale winners while maintaining governance. This pilot → measure → scale approach reduces risk and speeds adoption.
Staff training matters. A few hours of hands-on training can unlock substantial productivity gains. Also, appoint clinical champions who understand both workflow and tech. Their involvement helps to address frontline concerns and to accelerate ai adoption. Additionally, set KPIs such as reduction in admin hours, net revenue cycle improvement, clinician satisfaction, and error rates. These metrics help leaders decide when to expand use cases across departments.
Use AI to enhance resource allocation. Reassign staff from low‑value tasks to complex coordination, patient outreach, or care navigation. Also, invest saved time into quality improvement projects. Remember to calculate transition costs and to design retraining programs. Leaders should also plan for continuous monitoring and improvement of models and for periodic audits.
For ops teams that handle many emails and data sources, no-code AI email agents reduce response time and errors. For logistics-style tasks inside health systems, our solution helps integrate ERP and email context so teams work faster. To learn more about using AI for email drafting in operational contexts, see our piece on AI for freight forwarder communication for techniques that translate to health settings (AI for freight forwarder communication). Also, explore how automating logistics emails with Google Workspace and virtualworkforce.ai can map to clinical inbox triage (automate logistics emails with Google Workspace).
Finally, remember that the value of AI depends on responsible design, clinical buy-in, and ongoing governance. When you harness AI correctly, teams will work smarter, patients will see faster service, and health care costs may fall. Therefore, take measured steps to adopt AI and to scale what works.
FAQ
What specific administrative areas in a health system can AI improve?
AI can improve documentation, billing, scheduling, claims processing, and patient communications. Additionally, AI can help triage inbound messages and summarize clinical encounters so staff spend less time on routine clerical work.
How much time can AI realistically save clinicians and staff?
Pilots demonstrate meaningful savings. For example, a recent study noted roughly 122 hours per worker per year in some admin tasks. Actual savings vary by workflow, but many organizations report weeks saved annually per employee when they automate repetitive tasks.
Are there concrete AI tools suited for clinical documentation and billing?
Yes. Tools like Dragon Medical One speed note capture via speech-to-text, while RPA platforms automate billing steps. Also, ai-powered email agents can draft context-aware replies and update systems. Choosing the right ai tool depends on integration needs and governance requirements.
How do we measure success for an AI pilot in the health system?
Measure hours saved, claim denial rates, appointment fill rates, clinician time with patients, and clinician satisfaction. Also track error rates and escalation volumes. These metrics create an actionable business case for scale.
What governance steps reduce risks with AI in healthcare?
Governance should include testing on representative datasets, audit logs, human-in-the-loop rules, role-based access, and incident response plans. Additionally, maintain transparency about model behavior and keep clinicians involved in validation.
Can AI replace clinical judgment?
No. AI is best used to augment clinicians by handling routine administrative tasks and suggesting actions. Humans must retain authority for diagnosis and treatment decisions, especially in ambiguous or high-risk cases.
How does AI affect workforce planning in administrative roles?
AI shifts some routine duties away from staff and creates opportunities to redeploy employees into higher-value roles like care coordination. Planning should include retraining and clear role redesign to capture the benefits of automation.
What privacy concerns arise with AI in healthcare?
Privacy concerns include handling sensitive information and ensuring secure access to patient records. Use role-based controls, redaction, and strict logging. Also ensure vendors comply with healthcare privacy standards and perform regular audits.
How do we choose between no-code AI options and custom development?
No-code options speed deployment and reduce reliance on AI training specialists, while custom builds offer fine-grained control. Choose based on integration needs, governance capacity, and the complexity of the workflow you want to automate.
Where can I learn more about practical AI email automation for operations?
For operational email automation strategies that translate to health settings, review real-world guides such as virtualworkforce.ai’s resources on automated logistics correspondence and on how to scale operations with AI agents. These resources show how integrated connectors and email memory improve speed and accuracy in high-volume mailboxes.
Drowning in emails?
Here’s your way out
Save hours every day as AI Agents label and draft emails directly in Outlook or Gmail, giving your team more time to focus on high-value work.